A Dramatic Shift In Healthcare
Sometimes, statistics and data can be very insightful. Recently, one of our patients posted an interesting graph on his Facebook page reflecting one such example:
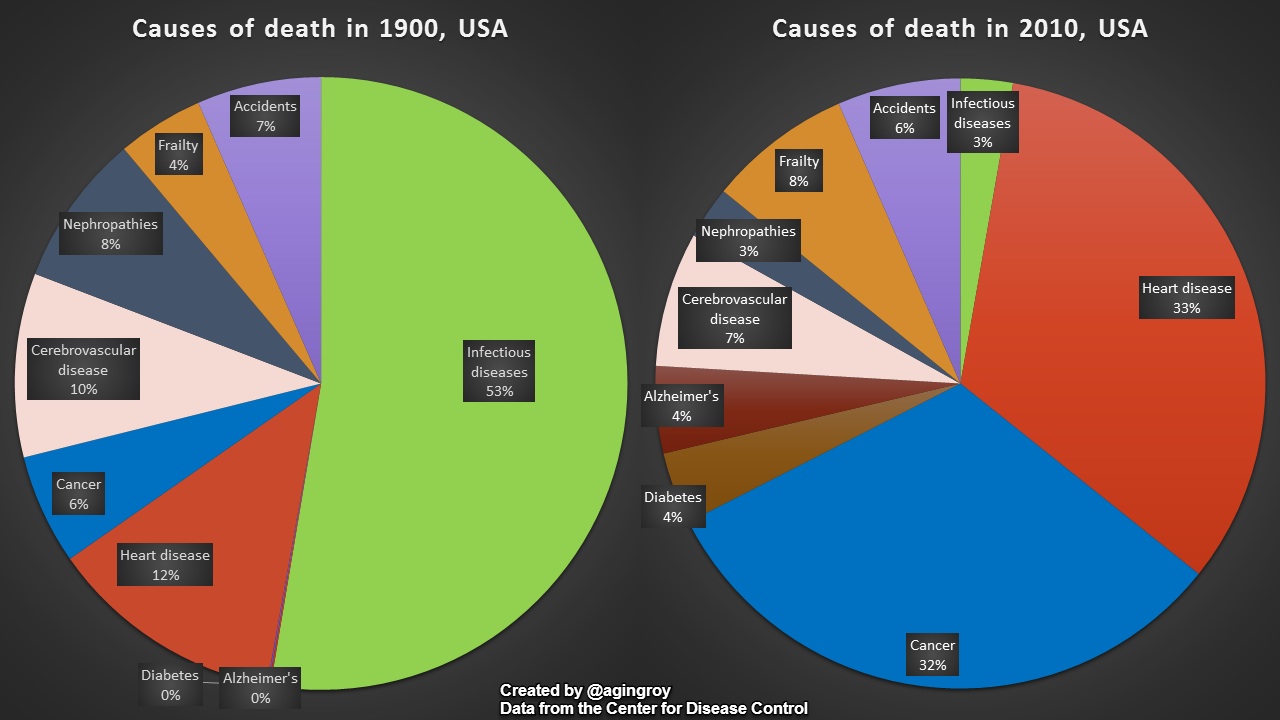
While this graph compares a whole century of evolution in medical care, encompassing a multitude of factors, most notably the discovery of antibiotics, the fact of the matter is that this graph can be summarized by a simple conclusion: causes of death have dramatically shifted over the last century from acute, infection-based conditions now to chronic, inflammatory disease-based conditions. Deaths due to infections have nearly evaporated from 53% down to a barely noticeable 3%, while the collective group of cancer, heart disease, diabetes, and Alzheimer’s disease have ballooned from 18% to 73%.
What does this say about the health of society, and more importantly, what does this mean to each of us as individuals? We’ve done a good job at identifying and treating acute and potentially threatening infections. We’re living longer, and subsequently, we need to take better care of ourselves in areas that are harder to assess and harder to continuously be attentive toward. Because it’s now even less of a race and even more of a marathon, we need to pay continuous and disciplined attention to our form – to the basic fundamentals of our body and it’s performance, and not just react when emergent symptoms arise, which can commonly reflect a crisis point. Think about it: how do we measure “inflammation”, the now-understood common basis of heart disease, diabetes, and more? Sure, there’s the cardiac CRP blood test, but how accurate is this in truly assessing inflammation? And of course, historically, there’s profiling each individual’s risk factors – but just how helpful is this? And when do we really become more aware that inflammation is an issue? – commonly, it’s when we’re diagnosed with diabetes, a stroke, or a heart attack: the latter stages of disease. And thus, we arrive at this conclusion: it’s time to stop just giving lip service to “preventive medicine”, and actually put it into action.
So, what can we do? At a minimum, this should urge us to continue, or increase, our mindful nutrition and exercise habits. Eating healthily (fruits and vegetables; living foods rather than processed foods) and exercising regularly go a long, long way in keeping our bodies clean and optimally fueled. Further steps might include awareness and reduction of toxins that burden our bodies: cigarettes, alcohol, heavy metals from our water source or other foods (eg, mercury in certain fish), plastics in our food preparation or storage (eg, BPA in food containers), environmental influences at some of our workplaces, stress management (which may include relationship conflicts, internal conflicts, life circumstances of which we have less influence, etc), and more. Quantified diagnostic steps might include specialized functional testing: assessing our gut health ecosystem (healthy, balanced bacterial colonies? unwanted yeast or parasites? malabsorption or digestive deficiencies?), our micronutrient cellular energy-production processes (adequate anti-oxidants, B vitamins, and other minerals that allow our bodies optimal fuel for performance?), food intolerances/allergies, and hormonal imbalances (thyroid, adrenals, gonadal organs?).
At Personal Care Physicians of Greater Newburyport, we are dedicated to engaging with our patients to dig as deep as you are willing to go, and help you take whatever action you’re ready for at any given moment, allowing you to experience life to its fullest for as long as possible. Let’s make life less about avoiding disease and more about pursuing vitality!
